Storygram: Anna Maria Barry-Jester’s “Surviving Suicide In Wyoming”
Editors’ note: We are saddened by the recent suicides of Kate Spade and Anthony Bourdain. This Storygram was written and readied for publication before their deaths, and we feel that the best way to honor them, as well as the scores of not-famous people impacted by suicide and mental illness, is to publish. The more people who read and think about the important issues raised in Barry-Jester’s piece, the better. For more information on reporting on suicide, read this.
The Storygram series, in which professional writers annotate award-winning stories to illuminate what makes a great science story great, is a joint project of The Open Notebook and the Council for the Advancement of Science Writing. It is supported by a grant from the Gordon and Betty Moore Foundation.
Anna Maria Barry-Jester is on the staff of the data-driven news site FiveThirtyEight where she covers public health, immigration, food, and science. This annotation was done by David Wolman and is co-published at The Open Notebook.
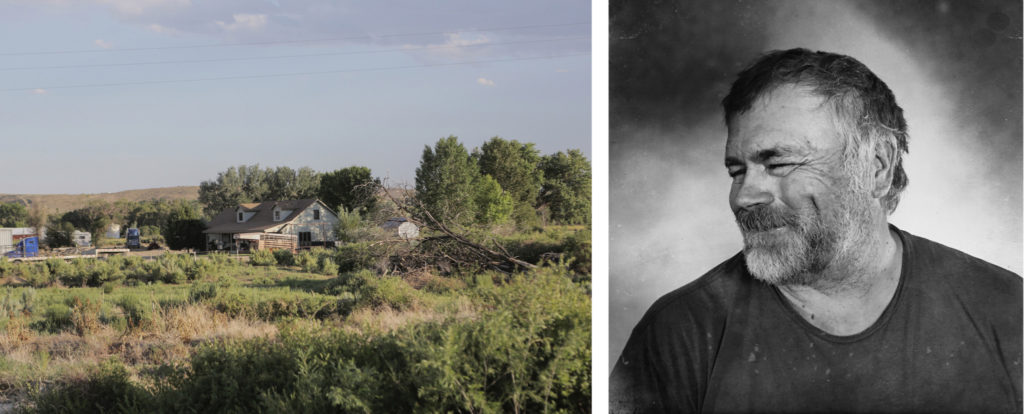
Kenny Michelena is, by just about any measure, a tough guy. He was born and raised on a ranch in rural northwestern Wyoming and remembers that after class in elementary school, the bus driver would drop him off wherever he saw the family tractor, so he could go straight to work in the fields. He worked just about every day of his life from the age of 8, first lambing sheep and plowing fields, later helping run the farm. In his 30s, when the ranch became unprofitable in a shifting economy, he drove trucks packed with cattle and other animals across the country, backbreaking labor that put him on the road for weeks on end.
Then, several years ago, the pain started. It began in his shoulder, but it quickly took over his whole body, preventing him from working. There were days when he could hardly get off the couch. “I was raised where your pride, your reason for being alive was work,” Kenny said.

He went to several doctors, and none could find anything wrong with him. He remembers one telling him he was just an overweight truck driver looking to collect disability.
It wasn’t until early in 2014, when he consulted a physician assistant in a nearby town, that he started to get some answers. The physician assistant said she’d do the X-ray, but she also wanted to draw blood. Test results showed that he had hemochromotosis, a genetic condition that causes excess buildup of iron in the body, which can lead to liver and heart failure, among many other life-threatening concerns, if left untreated.
NATIONAL ACADEMIES KECK FUTURES INITIATIVE COMMUNICATION AWARD |
| The Keck awards promote effective communication in science, engineering, medicine and any interdisciplinary work within and beyond the scientific community. This story won in the online category in 2017. |
“Maybe in a bigger town, or with more doctors, that wouldn’t have gotten so bad,” Kenny, now 58, said recently from a reclining chair in his living room, looking out through the kitchen to the fields and mountains in the distance.
The diagnosis brought Kenny some solace, but the searing pain remained. It was just one of the many problems swimming around in his head, pulling him deep inside himself that summer. The aching wouldn’t let him sleep or work, so his schoolteacher wife, Lisa, was supporting them. And there was the family ranch that he and his brother had different ideas about how to manage but could both agree probably wouldn’t turn a profit again. He began to worry about money. He thought, as he sometimes had since he was a teenager, about using one of the dozen of guns he keeps at home to end his life.
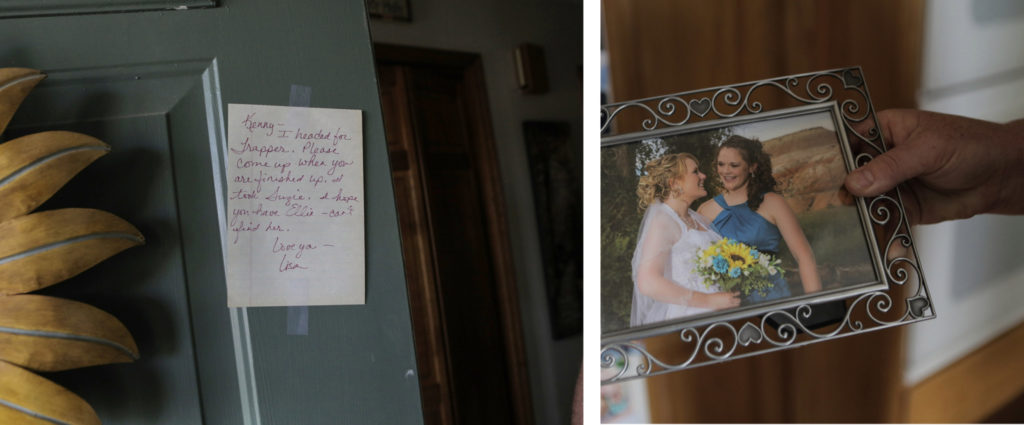
One of his two daughters, the one still living at home, got married and moved away. He knew that would hurt emotionally, but it was worse than he had anticipated. “Nobody wants to see their kids go, but I’d been dreading it since the day they were born,” Kenny said. He made it through her wedding and then brought his other daughter’s beloved animals to the state fair a few weeks later — the sisters had been state champions a few times; he didn’t want to disappoint them. “I held up long enough to get those two things done, and then I just let go,” Kenny said.
He woke up early one morning in August to do a day’s work for the local agriculture cooperative, but he never made it. Kenny told Lisa that he loved her, but he thought they’d be better off without him; he couldn’t take the agony anymore and wanted to end his life. Lisa called a crisis hotline, and then put Kenny in the car and drove him three hours from their rural home to the hospital in Billings, Montana.

As a middle-age white man living in the mountains of the Western United States, Kenny is among the demographic of Americans most at risk for suicide in the country. With a suicide rate of 44 per 100,000, men in this age and geographical group have more than three times the risk of dying by suicide than the national average. In Wyoming, approximately 80 percent of suicides are men; a quarter are men ages 45-64.
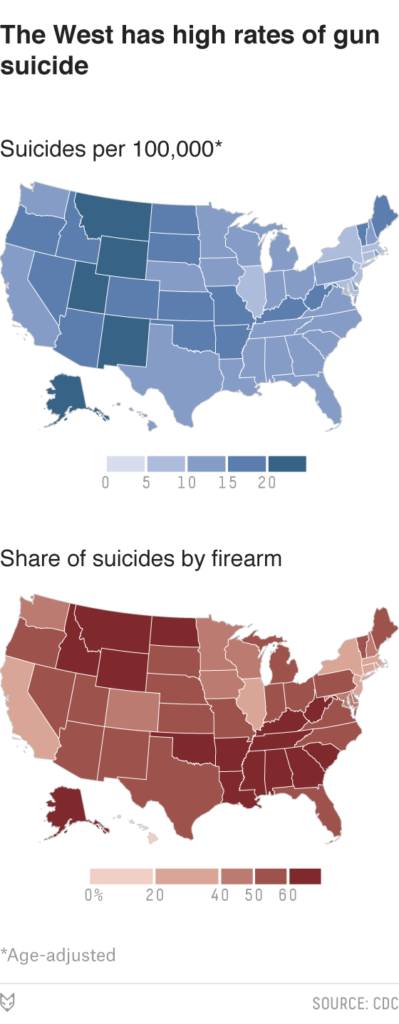
Though firearms are the third-most common method for attempting suicide, they are responsible for the largest share of suicide deaths because they are so lethal. Nationally, nearly two-thirds of all deaths by firearm are due to suicide, and Wyoming has had the highest rate of suicide by firearm of any state over the last 15 years. Studies have linked higher rates of gun ownership with increased risk of suicide death, but in Wyoming, which also has one of the highest rates of gun ownership in the country, this is an unpopular topic. As Tom Morton of the Casper Star-Tribune put it in a series of articles about Wyoming’s suicide epidemic, guns and suicide are the “third rail of Wyoming culture.”
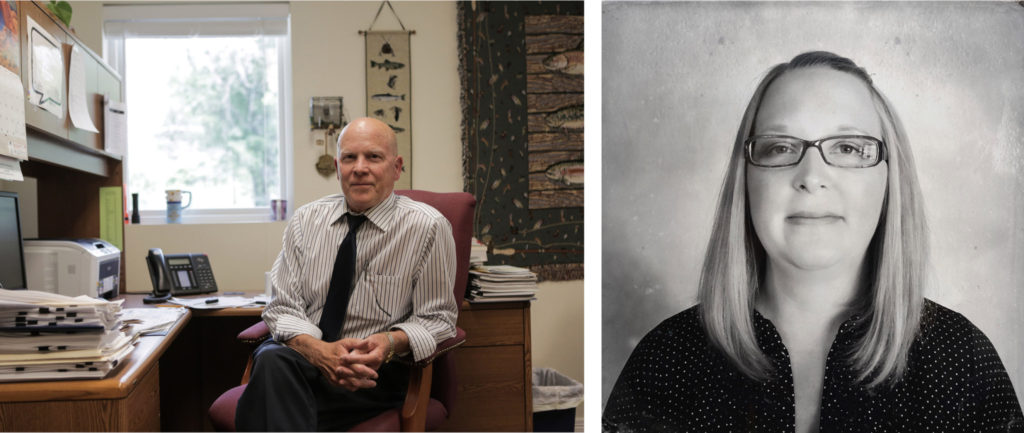
The high suicide rate isn’t news in Wyoming. “It’s certainly not going down this year. There’s a ton of concern, and nobody has any good answers,” said Mark Russler, the executive director of Yellowstone Behavioral Health Center, a community mental health program in Cody. Russler is responsible for much of the community mental health work in northwestern Wyoming. Despite more than a decade of concerted efforts to reduce the suicide rate, it continues to rise in the Mountain West. But that’s true all over the country — in every region, among every age group under 75, and among nearly every racial and ethnic group.
Local culture is a common explanation for the high rate in the West. In Wyoming, people call it the “cowboy-up” mentality — the get-your-shit-together, pull yourself up by your bootstraps, can-do attitude that they say is bred into children from a young age. That self-reliance helps people thrive in a landscape that’s big and tough, said Russler, but can also put them at risk if they get into a personal crisis.
Comparing health statistics in Wyoming to those from states in other parts of the country can be difficult because the population is so tiny (people describe the state as “a small town with a long main street”). But the trend in the Mountain West as a whole is clear, according to Carolyn Pepper, a professor of psychology at the University of Wyoming. She recently took a sabbatical to study why suicide is so common in the Western mountain ranges; using data from the Centers for Disease Control and Prevention’s Multiple Cause of Death database, she calculated just how bad the problem is and what might be causing it.1 Suicide rates have been higher here than in other regions for nearly a century, and while the rates are highest for middle-age white men, they are elevated for all sexes, races and ethnicities, especially American Indians, compared to their counterparts in other parts of the country.
“I kept hearing, as I talked to people out here, that it’s all about white men in rural areas, middle-age white men. And it’s true that, statistically, that’s the group most likely to commit suicide,” Pepper said. “But when you start looking at the data, this region of the country leads for men, for women, across all racial groups, across all ethnicities. It’s not just a rural problem, whatever it is is also in urban areas, as well as everywhere in between and across all age groups.”
Pepper thinks that means experts need to look beyond just white men and see what regional factors might explain the problem. Rurality is certainly one, as is the isolation that goes with it; Wyoming is nearly twice the size of New York state but with only 586,000 residents has less than 1/30th the population. She also notes that self-reported depression isn’t higher in the mountains, but alcohol and drug abuse are. Unemployment and low income are associated with high risk of suicide; Wyoming’s employment rate withstood much of the recession of the 2000s, but a recent drop in the prices of oil and minerals, which form the foundation of the state’s economy, is starting to wreak havoc on the finances of many families. There’s also the high rate of gun ownership.

After the brief hospital stay and months in therapy, Kenny said many of his life worries are still there, but things are very different today. “I can say right now that I’m better today than I was two weeks ago,” he said. “It’s hard to explain, it’s like I had to restructure my life. It took a lot of people a lot of time, but I’m happy to be alive.”
He said a lot of support has come from his family, even if they didn’t understand what was going on at times. He joined a church last year, and has spent time with the pastor, with whom he hit it off immediately and now counts as a friend. He was prescribed a few different regimens of medicine to help with his anxiety and depression, and feels lucky he found the right combination and dosage, since previous medications hadn’t helped. Before that happened, he’d wake up in the middle of the night, filled with what he calls the doom and dread, a sick feeling in his stomach that wouldn’t let him sleep. “The first night I was in the hospital, that happened that night. And the next day, I saw a doctor up there and she put me on some different medication, and that waking up, that never happened again,” Kenny said.
Ashley Fauber has been Kenny’s therapist since right after the event; after Kenny was first released from the hospital, he made the three-hour round trip drive from his rural home to Cody several times a week to see her as part of an intensive therapy program. Fauber said she often asks patients, “What made you come through my door? Because my door isn’t easy to come through.” Like Kenny, a lot of her patients are used to figuring out their own problems, never asking for help. Kenny said later if it hadn’t been for his wife and daughters, both their support and his desire to be there for them, he never would have made it that far.

Efforts to prevent suicide mostly fall in three broad categories: means reduction, which lowers the likelihood that someone in crisis will have access to a way to harm herself; awareness, so that people know where to get help and the general public knows how to spot someone in crisis; and perhaps most important, changing health care, by training primary care physicians to recognize symptoms of depression and mental illness as well as improving mental health treatment so that people don’t reach a point of crisis.
Some of the efforts around awareness, such as billboards and hotlines, have shown little success in Wyoming. A 2009 study found that such efforts may increase awareness but they appeared to have no effect on reducing suicide or getting more people to seek treatment. Another found that teenagers felt less likely to seek help if they had seen a billboard. Russler said his organization handled the calls from a hotline set up a few years ago, and just 12 phone calls were received over the six months that it ran in Park County (he also notes that none of those people actually came in for services). “We’ve thrown a ton of money at suicide prevention; all the attempts to increase awareness, media campaigns. That’s come and gone, and it hasn’t made a dent,” he said.
Reducing access to lethal means is one of the few tactics that has been shown to prevent suicide at a population level, either by making it more difficult to get a hold of a highly lethal method or by making that method less lethal. For example, particularly lethal pesticides were restricted in Southeast Asia, and the quantity of carbon monoxide in residential gas was reduced in the United Kingdom. But reducing the risk in that way isn’t always straightforward. In a state such as Wyoming, where firearms were involved in the largest share of deaths but are widely owned and used, it is a particularly complicated topic.
There is a well-established relationship between individual firearm ownership and suicide by firearm. More guns per household at the state level was also a strong predictor of suicide rates for both men and women, according to a May study from Boston University that looked at data from 1981 to 2013. Gun rights advocates have made the case that people will find an alternative method if a firearm isn’t available. And a 2008 survey commissioned by the state of Wyoming found that three-quarters of residents didn’t believe that reducing access to firearms can impact the state’s high suicide rate.
Need Help? |
| Call the toll-free National Suicide Prevention Lifeline at 1-800-273-TALK. |
While the research on the subject is mixed and very limited, it appears likely that suicide attempts are impulsive acts that can be prevented sometimes if the means of a planned attempt are taken away. And because other means are less lethal, not having access to a firearm can still be lifesaving, even if an attempt does take place. About 70 percent of survivors won’t go on to attempt suicide again, and 90 percent won’t die by suicide, according to a Harvard review of studies on survivors. That applies not only to firearms but to other methods, as well.
“We know [that] when people are in crisis, they use the method that is available to them,” said Terresa Humphries-Wadsworth, director of suicide prevention programs for the Prevention Management Organization of Wyoming, which manages all community suicide prevention efforts for the state. “If you remove one of those methods, whether that’s the pills or whatever, then they are less likely to go out and seek an alternative method, because they aren’t very good at problem-solving in that crisis moment.”
Those trying to address suicide in Wyoming say that national conversations about gun control often hurt local efforts to reduce access to firearms for people in crisis. BJ Ayers, a mother of three and the founder of Grace for 2 Brothers, a nonprofit organization in Cheyenne that works on suicide prevention, has made suicide prevention her life’s work. “I don’t want to take your guns away; I want to make sure that the gun is not accessible to a person when they are in a mental health crisis,” Ayers said. It’s been hard for her to get people to see the difference.
Gun violence is a deeply personal topic for her. In 2005, her youngest son took his life. Four years later, her middle son did the same. Both young men used firearms. Ayers and her organization have spent the last 10 years trying to beat back the suicide rate by building support networks for survivors, educating the community on suicide and holding an annual walk to raise awareness in hopes that the numbers will drop. “When we talk about gun violence, I just ask that we put our political views aside, and realize that this is a conversation about access to lethal means for someone who is in a mental health crisis; it has nothing to do with control,” Ayers said.
At his first appointment, Fauber asked Kenny whether he had any guns at home. He has a beautiful wood and glass gun case, which he made, in the corner of the family’s sun porch, and another rifle case sits in the living room. He keeps one in just about every vehicle, another in the workshop. “I don’t go anywhere without my gun. I rarely use it, but I guess it’s habit,” Kenny said later.

Out the front windows of Kenny’s cabin-style home, across a winding gravel road and a handful of other ranches, lie the Big Horn Mountains. Hunting there for elk was the only vacation he remembers taking as a child. Recently, hobbling around on a broken foot that was crushed by a young horse, he said he’d spend all his time riding around out there if he could. Having a gun is practically a necessity for survival in that landscape, which is home to bears, mountain lions and coyotes.
Kenny told Fauber that he did have guns and reluctantly told her that he was still thinking about using them to harm himself. By his next appointment, he admitted to her that they weren’t out of the house. So she called the local sheriff and, along with several other officers, he went over and moved them to Kenny’s brother’s house. Fauber remembers how concerned Kenny was about whether he’d get them back. He still has trouble talking about it, even as he’s opened up about other aspects of his struggle with depression.
“Was it hard for me to admit that I wasn’t safe around my guns? Yeah, it was really hard,” Kenny said. After he was out of crisis, the guns were brought back. Today he has proudly holstered them in their display cases.
Even when someone has already shown himself to be suicidal, we aren’t always good at keeping him safe from lethal means. A recent study from the University of Colorado looked at suicidal individuals in seven states who had made it to an emergency room, and found that more than 50 percent hadn’t been asked whether they had a firearm at home, or any other lethal means of attempting suicide.2 “We are missing the chance to save a lot of lives,” the study’s author told Science Daily.
Russler said that more often than not, families are supportive of keeping firearms away from suicidal members. “A lot of times someone will tell us they don’t [have a gun], but then their family members will tell us, ‘Oh yeah, they’ve got a handgun in their truck, it’s loaded.’” He acknowledged that making it harder for someone to get their hands on a means of attempting suicide is incredibly important, especially in a place where people don’t readily seek help, but he doesn’t think gun control laws are the answer. “I would not be a proponent of reducing access to someone owning a firearm,” Russler said, although he is in favor of using the screening that’s already on the books to make sure suicidal people aren’t buying firearms,3 and more generally to keeping guns stored in a way that makes them harder to get when someone is in crisis.
Wyoming is handing out gun locks in some areas in an attempt to reduce immediate access to firearms. While it’s hard to reduce the lethality of a firearm, the gun locks add a step to overcome before someone is able to use one, much like storing it in a locked case and keeping the ammunition separate. But Pepper said it’s unclear how many barriers need to be in place to really reduce the risk; moving guns out of a room probably isn’t enough, but moving them out of the house might be. It’s unclear where gun locks fit on that spectrum.
The prevention programs in place in Wyoming, which mostly come from a database of evidence-based practices kept by the Substance Abuse and Mental Health Services Administration, have all been successful in small communities in research settings. They haven’t been deployed at scale, however, in a way that has reduced the rate of suicide. As the national suicide rate rises, officials in Wyoming hope they can change that.
In 2012, Wyoming began a statewide push to get people trained in QPR, which stands for Question Persuade Refer. The idea is that, as with CPR training (the similarity in the names is not a coincidence), if enough people in a community are trained to recognize the signs of crisis or suicidal behavior, then someone will be able to intervene and get a person to treatment before they harm themselves. Wyoming has gone all in on the program: It has the highest concentration of trainers for the program of any state, and Humphries-Wadsworth said more than 10 percent of adults in the state have been trained. However, the impact of the program isn’t clear yet, she said, and it will be several years before it is.
Like most things in Wyoming, mental health treatment is often far away for people in rural areas. Still, the state has a fairly extensive network of community mental health programs, most of which accept payment on a sliding scale. The most common problems that people seek treatment for are affective disorders, such as depression and anxiety and bipolar disorders, which account for nearly 30 percent of the problems patients in the program experience. Alcohol-related problems are next, making up nearly 18 percent. All of these disorders are associated with high rates of suicide.
In the northwestern corner of the state, Russler and his colleagues are testing the program that Kenny took part in, called Brief Intensive Treatment. The idea is to help prevent suicidal people from having long stays in a hospital, and to get them more targeted, intensive therapy that involves the whole family. The first published evaluation of the program found it to be more effective at treating patients than traditional intensive therapy programs, though further studies are needed to determine if, and how well, it’s working.
Russler said he feels good about the programs in place, but thinks the reason they haven’t reduced the state’s suicide rate is that the highest-risk people are often the hardest to reach. “When we can get people to us, to treatment, they usually do well,” he said. While some people question whether there are enough mental health providers in Wyoming, Russler suspects that’s not the problem. Sure, they could use more specialists, he said, but the real problem is getting people into the mental health system. “The people committing suicide, they’re the ones we’re not seeing.” That’s why he thinks changing local attitudes about seeking mental health care, which he said is often seen as a sign of weakness, is key.
Russler said he’d mainly like to see mental health professionals placed into primary care settings, such as family doctor’s offices, and primary care doctors that are trained in recognizing signs of depression and anxiety.
When Kenny was looking for the source of his shoulder pain, he went to several doctors, and he exhibited other kinds of distress that could have been recognized by a trained professional as clues that his mental health was not good: sleeplessness and anxiety, among many others. There’s evidence that this missing of signs is common with people who attempt suicide. A 2014 study examined the records of 5,894 people in seven states who died by suicide between 2000 and 2010. The researchers found that 83 percent of those people had received some sort of health care in the year leading up to their death (64 percent of those were primary care visits), yet only half had had a mental health diagnosis. While suicide attempts may often be rash, desperate decisions, the depression and anxiety that often lead up to them are not, particularly in adults.
“I wish you could have seen him then, so you’d know how far he’s come,” Fauber said recently, recounting Kenny’s progress. “He’s so much fun,” she laughed, musing that she could easily sit around and talk to him all day, every day. When he first saw her, he was reticent, and had a hard time opening up about himself, what he was feeling. He was deeply concerned about not being able to work and provide for the family, and overwhelmed by the dark feelings and physical pain he was experiencing. Fauber started working with him the way she does with most patients — by explaining how the brain works. “Everybody wants to know why they feel the way they feel. I will literally draw a brain on the board,” Fauber said.
Kenny slowly opened up about some of his traumas. He can talk about them now, though he isn’t totally sold on the idea that triggers from his childhood are affecting him today. He says he had a great childhood: His mom kept a big garden and had something freshly baked for him nearly every day when he got in from working. His father kept up to 1,200 sheep, sometimes lambing a hundred in a day during birthing season.
But he also acknowledges that there’s another side to his story. An alcoholic father who suffered from chronic pain that likely came from the same blood disorder that plagues Kenny. Hard work from an early age that sometimes leaves him longing for a childhood he never had. Multiple family members have been treated for depression. Kenny now sees the connection between those things and his own battles. “I still feel bad, maybe even ashamed, that I fight depression,” he said, but he also says he’s learning to accept that the chemical and emotional legacy isn’t something he can change.
Kenny’s youngest daughter recently came home with a tattoo. It is of a small semicolon on her ankle, a symbol that represents a movement to acknowledge mental health concerns and promote suicide prevention. She told him she was glad he put a semicolon in his life instead of a period.
Kenny hasn’t talked to many people about his struggles with depression. He hasn’t told his neighbors, and he chose to see a therapist in a town an hour and a half away because when he went to a center nearby, he was connected in one way or another to most of the people in the office. He was clear, however, that if he could help prevent someone else from getting into his situation, sharing his story would be worth it.
This article is part of our project exploring the more than 33,000 annual gun deaths in America and what it would take to bring that number down. Our podcast What’s The Point is highlighting the project all week.
A longtime contributor at Wired, David Wolman has also written for publications including The New York Times, The New Yorker, Outside, Nature, and Bloomberg Businessweek. His work has twice been anthologized in the Best American Science and Nature Writing series, and his Atavist Magazine feature about Egypt’s revolution was nominated for a National Magazine Award. A former Fulbright journalism fellow in Japan, he is the recipient of an Oregon Arts Commission fellowship, and he has published four nonfiction books: The End of Money, Righting the Mother Tongue, A Left-Hand Turn Around the World, and Firsthand. He is currently working on a book about cowboys (HarperCollins, spring 2019). Follow Wolman on Twitter @davidwolman.
You may view this story in its original format at FiveThirtyEight. David Wolman’s Q&A with writer Anna Maria Barry-Jester is at The Open Notebook.

